The Atrocity of Resident Work Hours
Sarah Kim
Introduction
Residency hours have historically been unethical, with residents often working 36 hours consecutively and over 90 total hours a week.1 This is equivalent to pulling an all nighter for a test, except every decision you make means life or death. Following the tragic death of Libby Zion in 1984, who unfortunately passed away from resident malpractice, efforts have been made to remedy this issue. In 2003, the Accreditation Council of Graduate Medical Education (ACGME) set an 80 hour maximum averaged over a 4 week period and limited consecutive duty to 24 hours with an extension of 6 hours for patient continuity and education (total maximum of 30 hours).2 Nevertheless, in comparison to an average worker’s 40 hour workweek with 8-12 hour shifts, the extremity of this schedule is clear. In addition, further progress has not been made to this day due to the controversy surrounding this topic. For example, in 2011, ACGME limited first year resident physicians’ work hours to no more than 16 consecutive hours. This was then overturned in 2017 due to mixed responses.3 While criticisms of work hour limitations have some merit, to protect both patients’ and residents’ health and safety as well as prevent further physician shortage, work hours should have even stricter limits than what is already being enforced, and alternative solutions should address the possibility of detrimentally impacting patient outcomes.
Dangers of Sleep Deprivation
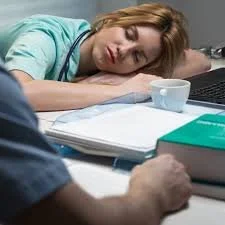
Studies show that the longer one stays awake, a person is subjected to increased frequency of microsleeps as well as lapses in cognition.4,5 Attention span, memory, motor function, mood are therefore impaired, which is extremely detrimental in a high-stakes medical environment.3 As aforementioned, in 2011, a law was instituted to implement a 16 consecutive hours limitation for first year resident physicians; however, this was overturned in 2017. A study comparing reported medical errors before (prior to 2011) and during the enforcement of the 16 hour limitation policy (2014-2017) revealed that the work hour limitation policy was correlated with a 32% reduced risk of physician-reported significant medical errors and a 63% reduced risk of medical errors resulting in fatalities.6 Clearly, these extreme work hours can seriously risk patient safety. Analogously, when examining the aviation field, pilots have had strict work hours and rest periods enforced since 1931 to prevent endangerment of pilots and passengers.7 If this is true for pilots, it does not make sense that greater limits have not been placed on the medical field as well.
Physician Shortage
With physician shortages, continuing to cultivate interest in medicine among younger generations is important; this interest is highly influenced by resident work hours. The physician shortage is a serious problem in the US. For one, the population is increasing in number and age, as fewer people are choosing to have children. From 2015 to 2030, the population aged 65 and older is projected to increase by 55%. As the number of older adults increases, the demand for health services is projected to increase as well.8 A 2017 projection for the annual physician workforce estimates a shortage of between 40,800 to 104,900 physicians by 2030.8 Thus, it is vital that interest in medicine is maintained throughout younger generations. A survey of 132 students from the New York University School of Medicine about “their attitudes towards work hour limitations and its effects on their interest in pursuing surgical residency” following the 1990 work hour limitations found that 95% of students believed it was a positive change due to varying reasons, with the most popular being better lifestyle and patient safety.9 Even more notably, 55% of students stated that work hour limitations were of higher importance than future salary.9 Hence, it is clear that work hour limitations can improve student interest in pursuing greatly needed medical careers.
Harmful Effects on Resident Physicians
Not only do the excessive work hours harm patients, they also are harmful to the physicians themselves. For example, Laura Barger, PhD, an associate physiologist in Division of Sleep and Circadian Disorders at Harvard Medical School, stated that working shifts of 24 hours or more is also correlated with an increased risk in a car crash after a shift, a significant cause for concern for the wellbeing of physicians.3,10 Furthermore, studies show that sleep deprivation causes people to “express a generalized excess of emotional sensitivity, with impairment in emotional discriminatory specificity.”5 The emotional control and empathy that these doctors have are essential for patient care, especially considering that it has been proven that compassion improves patient outcomes.11 With sleep deprivation directly correlating with a reduction in emotional regulation, extreme work hours not only further impact patients negatively but also have consequences on physicians' mental health and passion for their career.12 It is unethical to only consider patient outcomes and to disregard the physical and mental wellbeing of resident physicians.
Resident Hours Globally
The US lags far behind compared to other developed countries, having both an unmanageable workweek on top of 24-hour shifts.13 The European Union has requirements of a maximum work week of 48 hours and a minimum rest period of 11 consecutive hours per 24-hour duty.11 In Quebec, Canada, there is a 16 consecutive hour work limit.11 In Sweden, a maximum of 40 hours a week is required for residents. Despite these restrictions, there is no controversy or discourse about work hour restrictions in Sweden, with most believing that there is adequate training even with the work hour restrictions. This indicates Sweden’s success in implementing these restrictions. When residents in Sweden were interviewed, a common theme was that they believed that excellent content, organization, and supervision were more important than the quantity of hours, an important point to consider.14
Training of Residents and Patient Overload
While it seems simple to solve the above problems by reducing resident work hours, the difficulty comes in when considering the adequate training of residents. With our current model, residents learn through hands-on trial and error, often without sufficient supervision or structure. Additionally, they often lack the ability to focus and concentrate effectively due to sleep deprivation, reducing the effectiveness of their learning.13 However, because of the extreme work hours, residents are eventually trained to be successful confident doctors despite the lacking quality of learning.13 Thus, a problem that results from reduced work hours is that it can potentially prevent residents from gaining the adequate skills, confidence, and exposure they need to become a competent attending physician.11 A solution to resolving this issue is to compensate for the lowered hours of experience through a focus on quality of learning. Furthermore, another challenge to implementing reduced work hours lies in the shortage of physicians. With regulated hours for residents and physicians, the number of healthcare professionals needed to cover each day increases. If this increase in workers does not meet demand, both residents and attending physicians face a new problem of extreme workload per shift that limits learning, increases stress, and harms patient outcomes—similar to the problems resulting from sleep deprivation itself.15 Hence, an expansion of healthcare workers is essential to prevent reduced work hour policies from backfiring.
Recommendation
First, considering the vast negative effects on resident and patient health and safety, resident work hours should be limited to a maximum of 16 consecutive hours at least for first year residents, if not for all residents. After more than 16 consecutive hours of work, there’s a two fold increase in attention failures.16 Furthermore, we should be striving to aim for a 48 hour work week as other developed countries have already done. However, for now, a 60 hour work week is a doable transition for the US, considering the prevalence of large hospitals serving expansive populations as well as the shortage of physicians.
To address concerns about resident inadequacy that results from reducing work hours, resident programs should focus on improving the overall quality of resident learning. For one, resident programs should restructure to emphasize reflection periods to learn from training and also ensure adequate supervision. In addition, a study on internal medicine residents found that 9% of resident time was spent on indirect patient care that could be completed by other health care workers.17,18Another study found that 50% of resident shift time was used on computers, doing activities such as documentation.19 Hence, it is possible to focus resident time on learning medicine by optimizing online EMR systems and expanding medical teams within hospitals. On top of this, the reduced work hours will automatically improve the quality of resident learning by enabling residents to get adequate rest, which improves cognitive function, focus, and motor skills. Consequently, these changes to structure, supervision, focus on learning, and adequate rest within resident programs will ensure that residents can become competent physicians, despite reduced working hours.
For the problems of patient overload and physician shortages, the US must focus on investing funds to expand medical schools, both in number and acceptances, as well as welcoming foreign medical school graduates. For example, in the UK, the number of senior doctors increased by 60% from 2000 to 2010 simply by expanding the number of medical schools and actively recruiting foreign medical school graduates.13 In addition, as previously discussed, by reducing resident physician hours, more interest can be cultivated in the medical field, which in itself further serves to resolve the shortage.
Once these recommendations are made into policy, funds must also be allocated towards ensuring implementation, such as through hiring a third party to conduct inspections on resident programs as well as charging fines to noncompliant programs, as New York did to enforce its 1998 resident work hour policy.20
Conclusion
If the US can realize that residents are also humans that deserve a manageable lifestyle, it is certainly possible to allocate some of its funds to fix these inhumane conditions by expanding the healthcare workforce, improving EMR systems and resident programs, and enforcing policies on resident work hours—ultimately benefiting us all.
References
- Imrie, K. R., Frank, J. R., & Parshuram, C. S. (2014). Resident duty hours: past, present, and future. BMC medical education, 14 Suppl 1(Suppl 1), S1. https://doi.org/10.1186/1472-6920-14-S1-S1
- Wilson, Michael R. “The New ACGME Resident Duty Hours: Big Changes, Bigger Challenges.” The Ochsner Journal, vol. 5, no. 2, 2025, p. 3, pmc.ncbi.nlm.nih.gov/articles/PMC3399327/. Accessed 23 Apr. 2025.
- “Limiting Resident-Physician Work Hours Improved Patient Safety Outcomes.” Sleep.hms.harvard.edu, sleep.hms.harvard.edu/news/limiting-resident-physician-work-hours-improved-patient-safety-outcomes.
- Durmer, J. S., & Dinges, D. F. (2005). Neurocognitive consequences of sleep deprivation. Seminars in neurology, 25(1), 117–129. https://doi.org/10.1055/s-2005-867080
- Krause, A. J., Simon, E. B., Mander, B. A., Greer, S. M., Saletin, J. M., Goldstein-Piekarski, A. N., & Walker, M. P. (2017). The sleep-deprived human brain. Nature reviews. Neuroscience, 18(7), 404–418. https://doi.org/10.1038/nrn.2017.55
- Weaver, Matthew D, et al. “National Improvements in Resident Physician-Reported Patient Safety after Limiting First-Year Resident Physicians’ Extended Duration Work Shifts: A Pooled Analysis of Prospective Cohort Studies.” BMJ Quality & Safety, 10 May 2022, p. bmjqs-2021-014375, https://doi.org/10.1136/bmjqs-2021-014375.
- “Magazine - ALPA.” Www.alpa.org, www.alpa.org/news-and-events/air-line-pilot-magazine/alpa-fights-pilot-fatigue.
- Kirch, D. G., & Petelle, K. (2017). Addressing the Physician Shortage: The Peril of Ignoring Demography. JAMA : The Journal of the American Medical Association, 317(19), 1947–1948. https://doi.org/10.1001/jama.2017.2714
- Miller, G., Bamboat, Z. M., Allen, F., Biernacki, P., Hopkins, M. A., Gouge, T. H., & Riles, T. S. (2004). Impact of mandatory resident work hour limitations on medical students’ interest in surgery. Journal of the American College of Surgeons, 199(4), 615–619. https://doi.org/10.1016/j.jamcollsurg.2004.05.275
- Kowalenko T, Haas-Kowalenko J, Rabinovich A, Grzybowski M. Emergency medicine residency related MVCs—is sleep deprivation a risk factor? Academic Emergency Medicine 2000;7(5):451.
- Trzeciak, Stephen, and Anthony Mazzarelli. Compassionomics : The Revolutionary Scientific Evidence That Caring Makes a Difference. Pensacola, Fl, Studer Group, 2019
- Lingenfelser TH, Kaschel R, Weber A, Zaiser-Kaschel H, Jakober B, Kuper J. Young hospital doctors after night duty: their task-specific cognitive status and emotional condition. Medical Education 1994;28:566-572.
- Temple, J. Resident duty hours around the globe: where are we now?. BMC Med Educ 14 (Suppl 1), S8 (2014). https://doi.org/10.1186/1472-6920-14-S1-S8
- Sundberg, K., Frydén, H., Kihlström, L. et al. The Swedish duty hour enigma. BMC Med Educ 14 (Suppl 1), S6 (2014). https://doi.org/10.1186/1472-6920-14-S1-S6
- Peets, A., & Ayas, N. T. (2012). Restricting resident work hours: The good, the bad, and the ugly. Critical Care Medicine, 40(3), 960–966. https://doi.org/10.1097/CCM.0b013e3182413bc5
- Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, Rothschild JM, Katz JT, Lilly CM, Stone PH, et al.: Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med 2004, 351: 1829-1837. 10.1056/NEJMoa041404
- Alromaihi, D., Godfrey, A., Dimoski, T., Gunnels, P., Scher, E., & Baker-Genaw, K. (2011). Internal medicine residents' time study: paperwork versus patient care. Journal of graduate medical education, 3(4), 550–553. https://doi.org/10.4300/JGME-D-11-00057.1
- Knickman JR, Lipkin M, Jr, Finkler SA, Thompson WG, Kiel J. The potential for using non-physicians to compensate for the reduced availability of residents. Acad Med. 1992;67(7):429–438. doi: 10.1097/00001888-199207000-00003.
- Mamykina, L., Vawdrey, D. K., & Hripcsak, G. (2016). How Do Residents Spend Their Shift Time? A Time and Motion Study With a Particular Focus on the Use of Computers. Academic medicine : journal of the Association of American Medical Colleges, 91(6), 827–832. https://doi.org/10.1097/ACM.0000000000001148
- Poulose, B. K. , Ray, W. A. , Arbogast, P. G. , Needleman, J. , Buerhaus, P. I. , Griffin, M. R. , Abumrad, N. N. , Beauchamp, R. D. & Holzman, M. D. (2005). Resident Work Hour Limits and Patient Safety. Annals of Surgery, 241 (6), 847-860. doi: 10.1097/01.sla.0000164075.18748.38


U.S. medical residents’ extreme work hours are portrayed as unsafe and unethical because sleep deprivation increases medical errors and harms residents’ wellbeing, while also discouraging future physicians and worsening shortages. The piece recommends stricter hour limits alongside improved training structure and supervision, EMR/workflow optimization, workforce expansion, and stronger enforcement to prevent patient-care drawbacks.